The brain acronym tool helps a new parent make good, informed decisions in a high stress environment – labor and delivery. B.R.A.I.N. stands for benefits, risks, alternatives, intuition, and nothing. This tool helps parents get the information needed to make excellent decisions with their care providers during pregnancy, birth and postpartum. Parents that use the brain acronym get informed consent.
Pregnant women want their ideas, opinions, and questions to be heard and to be an integral part of the decision making process in regards to their care. Want to know the pros and cons of a labor in auction? Doulas, midwives, and other birth professionals can help parents use their BRAIN acronym tool to figure out what to do next.
On This Page
7 Minute Read
↓Why Does This Matter?
↓Assume Positive Intentions
↓Clarify the Problem
↓B.R.A.I.N. Acronym for Labor
↓B is for Benefits
↓R is for Risks
↓A is for Alternatives
↓I is for Intuition
↓N is for Nothing
↓N is for Negotiation
↓S is for Safe & Satisfying
↓Conclusion
↓Watch for Red Flags
Why Does This Matter?
Research has shown that the more a woman is part of the decision-making process during birth, the more she will be happier and more satisfied after her birth, no matter the type of birth or birth outcome.
“It is also suggested that active involvement of pregnant woman in decision-making process for the delivery method will increase the rate of vaginal birth after c-section and decrease c-section rate and improve the degree of maternal satisfaction after delivery.”
Plain and simple, if a woman is ignored and steamrolled, she will be unhappy about her experience giving birth. This dissatisfaction can have long lasting consequences in the way she mothers, her self-esteem, and future pregnancies.
Communicating birth preferences with care providers is a two way street and sometimes both parties lack the skills to come to the desired outcome. This blog post teaches the b.r.a.i.n. acronym tool on how to ask questions and get good information in order to make the best decision for each individual, their baby, and family.
Assume Positive Intentions
Before asking questions, sometimes it’s helpful to take a step back from a particular situation. I find it helpful to assume a doctor, midwife, or nurse’s positive intention. Most of the time an OBGYN, midwife, or nurse is not out to ruin your day or your birth. They are doing their best they can with what they know. Just as we are living our own lives the best we can the best way we know how, they are doing the same.
Clarify the Problem
After we assume their positive intention, our next step is to clarify the problem. For example, say your doctor or midwife suggests a labor induction. If you’re not sure, it’s a good idea to clarify the problem, if any. Upon asking what the problem is you might find out that your perception of the problem and what your care provider thinks might be two totally different things.
Because an induction was suggested, you might think that you or your baby is in danger. Your care provider might simply think that you’re sick of being pregnant and are anxious to get the show on the road, and is just trying to help. Upon further investigation, it would seem that your care provider is simply trying to be compassionate in their own way. Maybe there is not a problem at all!
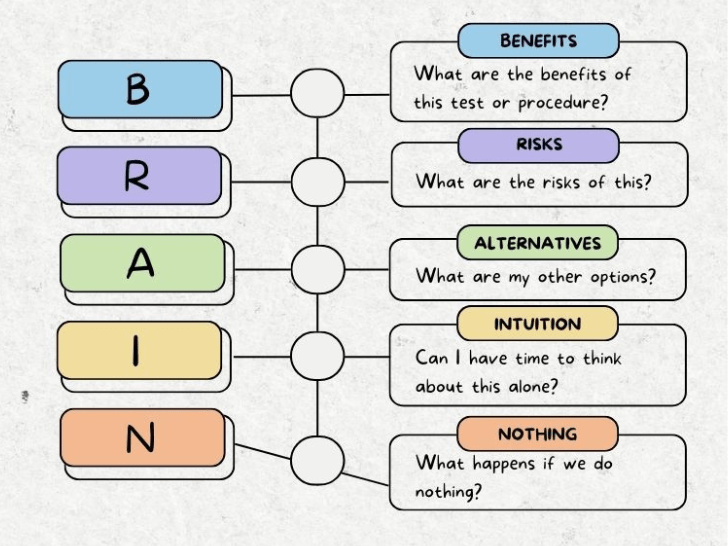
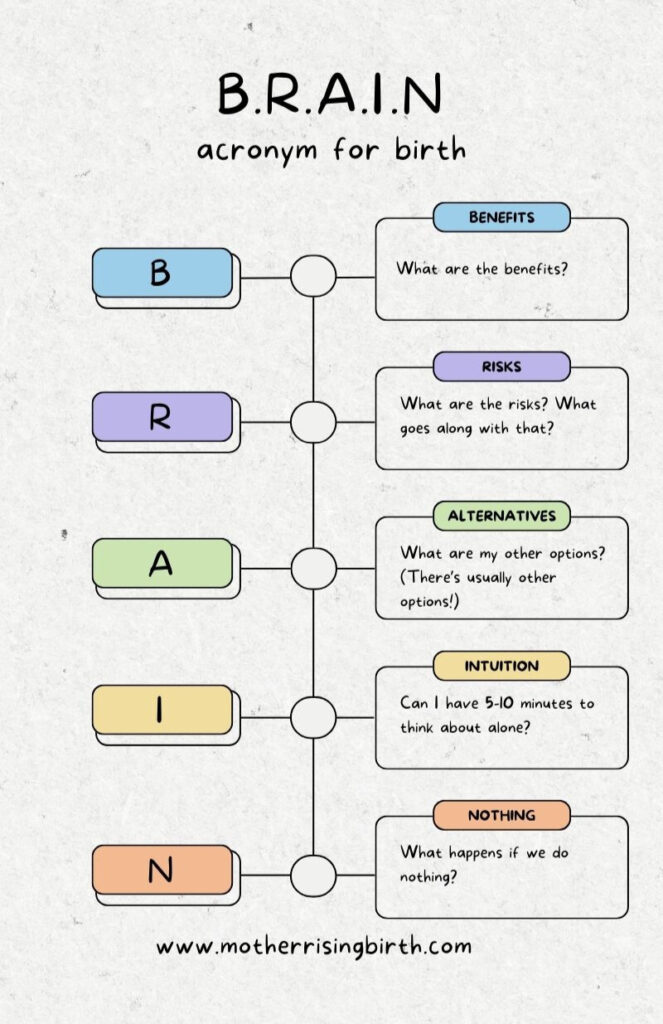
B.R.A.I.N. Acronym for Labor and Birth Decision Making
Let’s learn the B.R.A.I.N. acronym tool!
B – Benefits
R – Risks
A – Alternatives
I – Intuition
N – Nothing
N – Negotiation
B is for Benefits
“What are the benefits of this test or procedure?” or “How would this be helpful?”
R is for Risks
“What are the risks of this procedure?” or “What goes along with this test or procedure?”
A is for Alternatives
“What are my alternatives?” or “What are my other options?”
This is by far my favorite question to ask. This is also the question we impatiently skip to without doing the important work previously discussed. Make sure you take the time to get all the information!
I is for Intuition
“What is my intuition telling me?”
Ask for 5-10 minutes alone to talk it out with your partner and express yourselves freely. At this point you and your partner should check in with yourselves and each other to see what your gut, or intuition is telling you. Please know you can ask for time to talk… alone. If you want to clear a room quickly, just spread the word that you’d like a few minutes to pray about your decision. You’ll find that quite effective. 😉
N is for Nothing
“What happens if we do nothing?”
Another excellent question to ask, and one that’s often forgotten is what happens if we do nothing? Sometimes in the heat of the moment, in the exhaustion of labor, it feels like we need to do something. Sometimes, nothing needs to be done and things can be readdressed in an hour or maybe never.
N is for Negotiation
An additional “N” is negotiation.
Now that you’ve had a moment to take in all the information you’ve gathered, this is the moment where you and your care provider negotiate a decision that is as close to a win-win as possible. We’re looking for a safe and satisfying outcome!
S is for Safe & Satisfying
“Is this proposed test or procedure safe and will it leave me satisfied?”
Some add an “S” to the end of the brain acronym – B.R.A.I.N.S. – so parents remember to ask if a test or procedure is safe and satisfying. This question offers further clarity for parents making important decisions in labor.
Practice Using Your BRAINS in Labor
What I just covered is a popular activity I teach in my childbirth classes and it is always a fantastic conversation starter. To get good with this skill, practice a birth scenario with your partner, friend, doula, or family member. Practice makes perfect! Here are some practice scenarios:
- Labor induction for big baby
- Breaking water at 5 cm
- Breaking water at 9 cm
- Pitocin for immediate postpartum
- Schedule cesarean birth for breech baby
Practice Using the BRAIN Acronym with Mother Rising
Let’s practice together! Our pretend scenario is the proposal of a labor induction.
“I would like to schedule you for a labor induction.” – Care Provider, MD
BENEFITS
Pregnant Person: “What are the benefits of this labor induction?”
Care Provider: “You will no longer be pregnant, uncomfortable, and will be able to hold your baby.”
RISKS
Pregnant Person: What are the risks of an induction? What goes along with that?
Care Provider: “An increased risk of cesarean birth, fetal distress, and vacuum extraction.”
ALTERNATIVES
Pregnant Person: What are my other options?
Care Provider: “We could wait another week and talk about it again and next week’s visit, but I worry that you’re becoming too uncomfortable.”
INTUITION
Pregnant Person: “I would like 10 minutes alone to pray/talk about this.
Care Provider: *walks out of the room so birth team can pray* 😉
NOTHING
Pregnant Person: “What happens if we do nothing?”
Care Provider: “Nothing. You and your baby are fine, other than being uncomfortable and not sleeping well.”
NEGOTIATION
Pregnant Person: “I would rather wait 2 more weeks to see if my labor starts spontaneously. After that we can talk about it again.”
Care Provider: “Waiting for spontaneous labor sounds great, but I would like to wait only 1 more week before re-visiting the prospect of induction, instead of 2.
CONCLUSION
Waiting one more week was agreed upon, and the induction topic will be revisited then. Both parties were heard, perspectives and opinions were taken into consideration, and a decision was made that both parties were happy with. This is a safe and satisfying option for the parents. Success!
Watch for Red Flags
Sometimes despite our most valiant efforts of effective communication, it becomes apparent that the dynamic between a care provider and parents-to-be is not working out. Any red flags and warning bells seen and heard should be noticed and addressed. If this is your situation, please consider firing your OB, even if it’s in mid to late pregnancy.
B.R.A.I.N. Acronym Tool: What do you think?
So, let’s not end the conversation here. I’d love to know what you think. So tell me, what is something that worked well when communicating with your care provider? How did you know it was working for you? Leave a comment and let us know!

Naomi Bradfute RN Nd
Wednesday 10th of April 2019
I have been a nurse for 30 years in various aspects of OB, mostly labor and delivery. This is awesome! Really well done. I wonder if you would address ideas for women who do not have options for different providers. There are many medically underserved areas of this country.
Sadoula
Saturday 6th of October 2018
In some institutions if you don’t go with the ob decision you are not treated with the same care and attention. Especially during labour.
Lindsey
Saturday 6th of October 2018
That's why it's so important to test the character of your care provider during pregnancy. We need to see what they're made of! Check out this post: https://www.motherrisingbirth.com/2018/10/fire-your-ob.html
Wendy
Friday 20th of July 2018
I’ve always heard and taught that the N in BRAIN was, ‘what if we do Nothing’ at this time. I like negotiation. I think that’s great, but with the understanding that even if your care provider encourages and wants you do do something, that you have the right to say NO. We choose to do nothing at this time! (Of course that is if both mom and baby are healthy and safety isn’t an actual reason for looking at doing something.
Lindsey
Monday 23rd of July 2018
I've heard various ways of doing the brain acronym as well. The thing is, I feel like the nothing question, can be asked in A - Alternatives. Doing nothing is an alternative, or another choice. Thanks for your comment! :)